As cold and flu season approaches, many people search for natural remedies to support their immune system and reduce the severity of symptoms. One popular option that has gained attention in recent years is elderberry. Elderberry for colds has been praised for its ability to boost immunity, shorten the duration of illness, and relieve symptoms of respiratory infections. Elderberries are rich in antioxidants, vitamins, and other compounds that can support the immune system, making them a valuable addition to any wellness routine. This article will explore the benefits of elderberry for colds, how it works to boost immunity, and how to use it as part of your health regimen.
What is Elderberry?
Elderberry comes from the Sambucus plant, a small shrub that produces dark purple-black berries. These berries have been used for centuries in traditional medicine to treat a variety of ailments, from colds and flu to inflammation and skin conditions. The elderberry plant, especially its fruit, is known for its medicinal properties, which are largely attributed to its high content of antioxidants, flavonoids, and vitamins.
Elderberries are particularly rich in vitamin C, which plays a crucial role in immune function, and anthocyanins, a type of antioxidant that helps to combat oxidative stress. Additionally, elderberries contain compounds that have antiviral properties, making them an attractive option for those looking to boost their immune system during cold and flu season.
How Elderberry Works for Colds
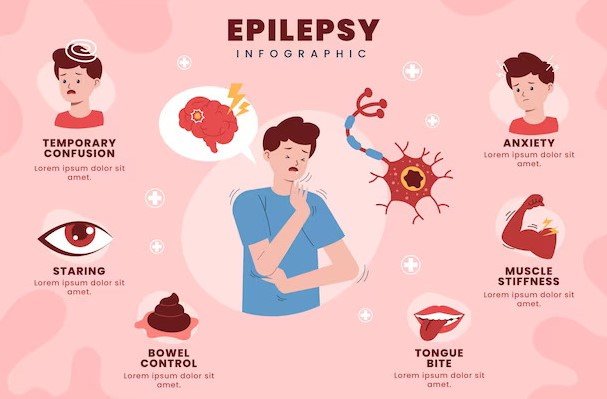
When taken during the early stages of a cold, elderberry can help to shorten the duration of symptoms and reduce their severity. There are several mechanisms through which elderberry for colds may exert its beneficial effects:
- Antiviral Properties: Elderberries have been shown to inhibit the activity of viruses, particularly influenza (flu) and other respiratory viruses. Studies suggest that elderberry may prevent the viruses from entering healthy cells, effectively stopping the virus from spreading within the body.
- Boosting the Immune System: Elderberry contains compounds that stimulate the immune system. These compounds help increase the production of cytokines, which are molecules that help regulate immune responses. By boosting immune function, elderberry may help your body fight off infections more effectively.
- Reducing Inflammation: Elderberry is known to have anti-inflammatory effects, which can be particularly useful for reducing symptoms like congestion, sore throat, and swelling associated with colds. By calming inflammation, elderberry can provide relief from the discomfort that often accompanies respiratory infections.
- Rich in Antioxidants: Elderberries are packed with antioxidants, such as anthocyanins, which help neutralize free radicals in the body. These antioxidants play a crucial role in protecting cells from oxidative damage, thus supporting overall immune health and aiding in recovery during illness.
The Health Benefits of Elderberry for Colds
Using elderberry for colds offers several health benefits that can help individuals recover more quickly and feel better during illness. Below are some of the most prominent benefits:
1. Shortens the Duration of Cold Symptoms
One of the key benefits of elderberry is its ability to shorten the duration of a cold. Studies suggest that taking elderberry extract within the first 48 hours of experiencing cold symptoms can significantly reduce the length of the illness. In a clinical trial, individuals who took elderberry syrup reported feeling better after an average of four days, compared to those who received a placebo, who reported symptoms for around eight days.
2. Alleviates Symptoms of Respiratory Infections
Elderberry has been shown to relieve symptoms such as congestion, sore throat, cough, and fatigue commonly associated with colds and flu. The anti-inflammatory properties of elderberry help reduce the swelling and irritation in the nasal passages, making it easier to breathe. Additionally, elderberry’s antioxidant content can help soothe sore throats and alleviate the discomfort caused by coughing.
3. Enhances Overall Immune Function
Regular consumption of elderberry can also improve your overall immune function, helping your body stay resilient against future illnesses. Studies have found that elderberry can boost immune system activity, making it a great addition to a preventative wellness routine, particularly during cold and flu season. It supports the production of cytokines and other immune cells, which help your body respond effectively to infections.
4. Supports Antioxidant Defenses
The high antioxidant content of elderberry provides additional protection for the body during cold and flu season. Antioxidants are important for neutralizing free radicals—unstable molecules that can cause cellular damage. By protecting your cells from oxidative stress, elderberry helps to maintain a healthy immune system, allowing you to recover from illness faster and reducing your chances of getting sick in the first place.
How to Use Elderberry for Colds
Elderberry can be used in a variety of ways to help alleviate cold symptoms and boost immunity. There are several different forms of elderberry available on the market, each offering a unique way to incorporate this natural remedy into your wellness routine.
1. Elderberry Syrup
One of the most popular ways to take elderberry is through elderberry syrup. This syrup is typically made from elderberry extract, water, honey, and sometimes additional herbs like echinacea or ginger. Elderberry syrup can be taken directly or added to warm beverages like tea or water. Most commercial elderberry syrups come with dosing instructions, but a typical dose for an adult is about 1-2 tablespoons per day for immune support or 1-2 teaspoons every 2-3 hours when fighting off a cold.
2. Elderberry Capsules and Tablets
Elderberry capsules or tablets are another convenient option for those who prefer a more straightforward, no-mess remedy. These are often standardized to provide a consistent dose of elderberry extract. Capsules can be taken as directed on the product label, typically once or twice a day, depending on the brand.
3. Elderberry Tea
Elderberry tea is another excellent way to enjoy the benefits of elderberry. Many brands offer dried elderberries or elderberry tea bags that can be steeped in hot water. For added benefits, you can combine elderberry with other immune-boosting herbs, such as echinacea, ginger, or lemon balm, to enhance the soothing effects of the tea.
4. Elderberry Gummies
For those who find it difficult to swallow pills or dislike the taste of syrup, elderberry gummies offer a tasty and convenient alternative. These gummies typically contain elderberry extract, vitamin C, and sometimes zinc, all of which contribute to immune support. The dosage varies by brand, so it’s important to follow the manufacturer’s instructions.
Potential Side Effects and Considerations
While elderberry is generally considered safe for most people when used as directed, there are a few things to keep in mind:
- Raw Elderberries: Raw elderberries, as well as other parts of the elderberry plant (including the leaves, stems, and seeds), contain cyanogenic glycosides, which can be toxic if consumed in large amounts. Cooking elderberries, as is done when making syrup or tea, removes these harmful compounds, making them safe to consume.
- Allergic Reactions: Although rare, some individuals may have an allergic reaction to elderberries. If you experience symptoms like itching, swelling, or difficulty breathing after consuming elderberry products, discontinue use and consult with a healthcare provider.
- Pregnancy and Breastfeeding: Pregnant and breastfeeding women should consult a healthcare professional before using elderberry, as there is limited research on its safety during these periods.
Incorporating elderberry for colds into your wellness routine can provide numerous benefits, from boosting immune function to alleviating the symptoms of respiratory infections. Whether you choose elderberry syrup, capsules, tea, or gummies, this natural remedy offers an effective, gentle way to support your body during cold and flu season. By harnessing the power of elderberry, you can strengthen your immune system, reduce the duration of illness, and recover more quickly from colds. As always, it’s important to consult with a healthcare professional before introducing any new supplement or remedy into your routine, especially if you have preexisting health conditions. However, for those looking for a natural, time-tested remedy, elderberry is a valuable tool for maintaining health and well-being throughout the year.