A torn chest muscle, medically known as a pectoral muscle strain or rupture, is a condition that occurs when the tendons or muscles of the pectoral (chest) region are stretched or torn. This can be caused by various factors such as excessive weightlifting, sudden movements, or direct blows to the area. Symptoms often include pain, swelling, bruising, and a decrease in chest muscle strength. Recovery from a torn chest muscle involves rest, physical therapy, and in severe cases, surgical intervention. It is a process that requires time and patience, with the focus on gradually restoring strength and function to the affected area.
Understanding Torn Chest Muscle: Causes, Symptoms, and Steps to Recovery
A torn chest muscle, medically known as a pectoralis major rupture, is a severe injury that can significantly impact an individual’s quality of life. Understanding the causes, symptoms, and steps to recovery can help those affected by this condition navigate their healing journey more effectively.
The pectoralis major is a large muscle in the upper chest, responsible for controlling arm movements such as pushing and lifting. A tear in this muscle typically results from excessive strain or a sudden, forceful movement. This injury is most common among athletes, particularly those involved in weightlifting, wrestling, and football, where intense physical exertion and contact are frequent. However, it can also occur in non-athletes due to accidents or falls.
The symptoms of a torn chest muscle are usually immediate and noticeable. The individual may experience a sudden sharp pain in the chest or upper arm, often described as a tearing or popping sensation. This may be accompanied by swelling, bruising, and a noticeable deformity in the chest muscle. The pain can intensify with arm movement, making it difficult to perform daily activities. In some cases, the individual may also experience muscle weakness or an inability to move the arm across the body.
Diagnosis of a torn chest muscle typically involves a physical examination and imaging tests such as an MRI or ultrasound. These tests can help determine the severity of the tear and guide the treatment plan. It’s crucial to seek medical attention promptly if a pectoralis major rupture is suspected, as delayed treatment can lead to complications and prolonged recovery.
The recovery process for a torn chest muscle depends on the severity of the injury. Mild to moderate tears may heal with conservative treatment, including rest, ice, compression, and elevation (RICE). Pain medication and physical therapy may also be recommended to manage pain and restore strength and flexibility to the muscle.
In the case of severe tears, surgical intervention may be necessary. This typically involves reattaching the torn muscle to the bone using sutures. Post-surgery, the individual will likely need to wear a sling for several weeks to immobilize the arm and allow the muscle to heal. Physical therapy will then be introduced gradually to regain muscle strength and range of motion.
Regardless of the treatment approach, recovery from a torn chest muscle requires time and patience. The healing process can take several months, and it’s essential to avoid rushing back into physical activities to prevent re-injury. Regular follow-ups with the healthcare provider are also crucial to monitor progress and adjust the treatment plan as needed.
In conclusion, a torn chest muscle is a serious injury that requires prompt medical attention. Understanding the causes and symptoms can help individuals seek timely treatment, while knowledge of the recovery process can set realistic expectations and promote effective healing. With the right care and commitment to recovery, individuals with a torn chest muscle can regain their strength and return to their regular activities.A torn chest muscle, also known as a pectoral muscle rupture, is often caused by excessive strain or injury during activities such as weightlifting or contact sports. Symptoms typically include sudden severe pain, swelling, bruising, muscle weakness, and a noticeable deformity in the chest muscle. Recovery involves rest, pain management, physical therapy, and in severe cases, surgical intervention. The healing process can be lengthy, often requiring several weeks to months. It is crucial to seek immediate medical attention if a chest muscle tear is suspected to ensure proper treatment and recovery.

 Painful pectoral muscle is a condition that affects the chest muscles, causing pain and discomfort. It can be caused by a variety of factors, including overuse, injury, or medical conditions. Symptoms of painful pectoral muscle can include pain in the chest, difficulty breathing, and difficulty moving the arms. Treatment for painful pectoral muscle typically involves rest, physical therapy, and medications. Recovery strategies may include stretching, strengthening exercises, and lifestyle modifications. This article will discuss the causes, symptoms, and recovery strategies for painful pectoral muscle.
Painful pectoral muscle is a condition that affects the chest muscles, causing pain and discomfort. It can be caused by a variety of factors, including overuse, injury, or medical conditions. Symptoms of painful pectoral muscle can include pain in the chest, difficulty breathing, and difficulty moving the arms. Treatment for painful pectoral muscle typically involves rest, physical therapy, and medications. Recovery strategies may include stretching, strengthening exercises, and lifestyle modifications. This article will discuss the causes, symptoms, and recovery strategies for painful pectoral muscle. Swollen knuckles can be a painful and uncomfortable condition that can affect anyone at any age. It is caused by a variety of factors, including injury, arthritis, and infection. Treatment for swollen knuckles depends on the underlying cause, but may include rest, ice, compression, and elevation. In some cases, medications or surgery may be necessary. It is important to seek medical attention if the swelling does not improve or if it is accompanied by other symptoms. This article will discuss the causes, treatment, and when to see a doctor for swollen knuckles.
Swollen knuckles can be a painful and uncomfortable condition that can affect anyone at any age. It is caused by a variety of factors, including injury, arthritis, and infection. Treatment for swollen knuckles depends on the underlying cause, but may include rest, ice, compression, and elevation. In some cases, medications or surgery may be necessary. It is important to seek medical attention if the swelling does not improve or if it is accompanied by other symptoms. This article will discuss the causes, treatment, and when to see a doctor for swollen knuckles.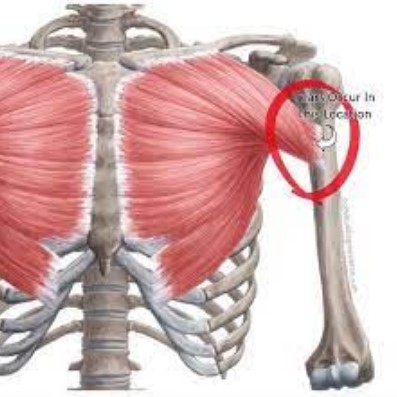 A torn pectoral muscle is a serious injury that can cause significant pain and disability. It is most commonly seen in athletes who participate in activities that involve pushing or pulling motions, such as weightlifting, football, and wrestling. The pectoral muscle is a large muscle located in the chest that helps to move the arm and shoulder. When it is torn, it can cause pain, swelling, and difficulty moving the arm. Treatment for a torn pectoral muscle typically involves rest, physical therapy, and possibly surgery. This article will discuss the causes, symptoms, and recovery strategies for a torn pectoral muscle.
A torn pectoral muscle is a serious injury that can cause significant pain and disability. It is most commonly seen in athletes who participate in activities that involve pushing or pulling motions, such as weightlifting, football, and wrestling. The pectoral muscle is a large muscle located in the chest that helps to move the arm and shoulder. When it is torn, it can cause pain, swelling, and difficulty moving the arm. Treatment for a torn pectoral muscle typically involves rest, physical therapy, and possibly surgery. This article will discuss the causes, symptoms, and recovery strategies for a torn pectoral muscle.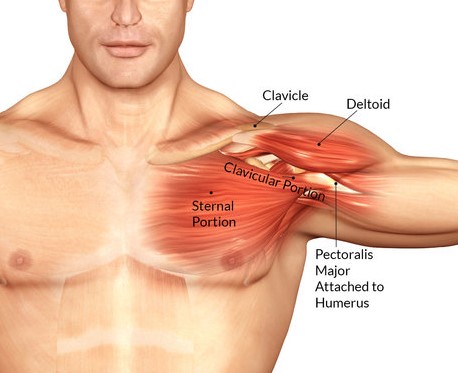 Torn Pec Recovery is a comprehensive guide to rehabilitation and healing after a pectoral muscle injury. It provides detailed information on the causes, diagnosis, and treatment of pectoral muscle injuries, as well as advice on how to prevent them in the future. It also offers practical tips on how to manage the pain and discomfort associated with a pectoral muscle injury, as well as how to speed up the healing process. With the help of Torn Pec Recovery, you can get back to your active lifestyle in no time.
Torn Pec Recovery is a comprehensive guide to rehabilitation and healing after a pectoral muscle injury. It provides detailed information on the causes, diagnosis, and treatment of pectoral muscle injuries, as well as advice on how to prevent them in the future. It also offers practical tips on how to manage the pain and discomfort associated with a pectoral muscle injury, as well as how to speed up the healing process. With the help of Torn Pec Recovery, you can get back to your active lifestyle in no time.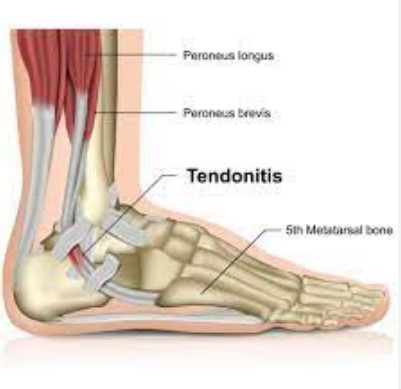 Torn ligaments in the top of the foot can be a painful and debilitating injury. The top of the foot is a complex area of the body, and the ligaments that support it can be easily damaged. Common causes of a torn ligament in the top of the foot include sports injuries, falls, and overuse. Treatment for a torn ligament in the top of the foot typically involves rest, ice, compression, and elevation. In some cases, surgery may be necessary. This article will discuss the causes of a torn ligament in the top of the foot, as well as recovery tips to help you heal quickly and safely.
Torn ligaments in the top of the foot can be a painful and debilitating injury. The top of the foot is a complex area of the body, and the ligaments that support it can be easily damaged. Common causes of a torn ligament in the top of the foot include sports injuries, falls, and overuse. Treatment for a torn ligament in the top of the foot typically involves rest, ice, compression, and elevation. In some cases, surgery may be necessary. This article will discuss the causes of a torn ligament in the top of the foot, as well as recovery tips to help you heal quickly and safely.