An Ear, Nose, and Throat Doctor, also known as an Otolaryngologist, is a specialist who diagnoses and treats conditions related to the ears, nose, and throat, as well as the head and neck. These medical professionals are skilled in managing diseases, structural issues, and injuries in these areas. It’s crucial to see an ENT specialist when experiencing persistent or severe issues such as chronic sinusitis, hearing loss, balance problems, throat discomfort, or voice changes. They also handle more complex conditions like tumors in the head or neck region. Timely consultation with an ENT specialist can lead to early diagnosis and effective treatment, preventing potential complications.
Understanding the Right Time to Consult an Ear, Nose, and Throat Doctor: When to See an ENT Specialist
Ear, nose, and throat (ENT) specialists, also known as otolaryngologists, are medical professionals who diagnose and treat conditions related to the ears, nose, and throat. These specialists are trained to manage diseases, abnormalities, and other health issues affecting the ear, nose, throat, neck, and head. However, many people are unsure when to consult an ENT specialist. Understanding the right time to seek help from an ENT specialist is crucial to ensure timely and effective treatment.
Firstly, persistent ear pain or discomfort is a clear sign that you should see an ENT specialist. This could be due to various conditions such as ear infections, hearing disorders, or even a foreign object lodged in the ear. If you experience symptoms like ringing in the ears (tinnitus), difficulty hearing, or a sudden loss of hearing, these could indicate serious issues that require immediate attention from an ENT specialist.
Secondly, issues related to the nose such as chronic sinusitis, nasal congestion, and nosebleeds are also within the purview of an ENT specialist. If you have been suffering from a stuffy nose for a prolonged period, or if you experience frequent nosebleeds, it is advisable to consult an ENT specialist. They can provide a proper diagnosis and suggest suitable treatment options.
Thirdly, throat problems like swallowing disorders, voice issues, or persistent sore throat also warrant a visit to an ENT specialist. If you have been experiencing a hoarse voice, difficulty swallowing, or a sore throat that doesn’t seem to go away, it’s time to see an ENT specialist. These symptoms could be signs of serious conditions like throat cancer or vocal cord paralysis.
In addition to these, ENT specialists also handle conditions related to the neck and head, including diseases of the larynx (voice box), thyroid, and parathyroid. They also manage disorders of the upper digestive tract and the trachea. If you have been experiencing persistent neck pain, swollen lymph nodes, or have difficulty breathing or swallowing, you should consult an ENT specialist.
Moreover, ENT specialists are also equipped to handle allergies. If you have been suffering from chronic allergies that lead to sinusitis, nasal congestion, or other related conditions, an ENT specialist can help identify the allergens and provide appropriate treatment.
Lastly, sleep disorders such as sleep apnea and snoring are also managed by ENT specialists. If you or your partner have noticed that you snore loudly, or if you wake up feeling tired even after a full night’s sleep, you might be suffering from a sleep disorder. An ENT specialist can diagnose the condition and suggest suitable treatment options.
In conclusion, an ENT specialist is a medical professional who can diagnose and treat a wide range of conditions related to the ears, nose, and throat. If you experience persistent or severe symptoms related to these areas, it is advisable to consult an ENT specialist. Early diagnosis and treatment can prevent complications and improve your quality of life. Remember, your health is your wealth, and timely medical attention is the key to maintaining it.In conclusion, one should consider seeing an Ear, Nose, and Throat (ENT) specialist when experiencing persistent or severe issues related to these areas, such as chronic sinusitis, hearing loss, balance problems, throat pain, or voice changes. ENT specialists are also necessary for the diagnosis and treatment of conditions like sleep apnea, tumors in the head or neck, or if you need surgery for an illness or injury affecting the ear, nose, or throat. Regular check-ups with an ENT can also be beneficial for maintaining overall health.


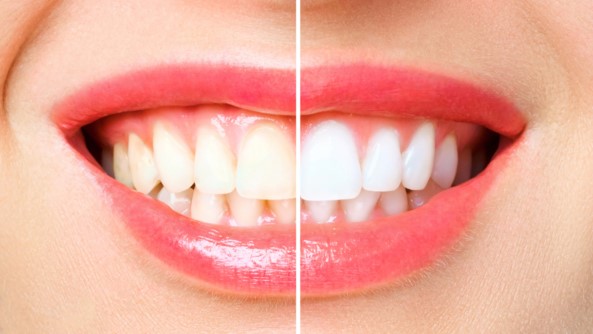
 Dental spacers, also known as orthodontic separators, are small devices used in orthodontic treatment to create space between teeth. They are typically made of rubber or metal and are inserted between the molars a week or two before braces are applied. The primary role of dental spacers is to move the teeth slightly apart so that orthodontic bands can be easily and accurately placed around the teeth during the next phase of treatment. These devices play a crucial role in preparing the mouth for braces or other orthodontic appliances, contributing significantly to the success of the overall orthodontic treatment plan.
Dental spacers, also known as orthodontic separators, are small devices used in orthodontic treatment to create space between teeth. They are typically made of rubber or metal and are inserted between the molars a week or two before braces are applied. The primary role of dental spacers is to move the teeth slightly apart so that orthodontic bands can be easily and accurately placed around the teeth during the next phase of treatment. These devices play a crucial role in preparing the mouth for braces or other orthodontic appliances, contributing significantly to the success of the overall orthodontic treatment plan.